A friend of mine called me the other day, to tell me that he used Healee, to see a doctor for one of his kids. He sounded quite happy with what he got, he wouldn’t stop talking about how easy and convenient it was.
“This Healee thing saved the day, I’m telling you! We got in touch with the doctor, sent pics of the rash on Victor’s arm, did a short video call, and the doctor then told me what to do. All that in less than 30 minutes! With my wife out of town that day, the little one being semi-sick, and me working on a super important project, I literally don’t know how I would squeeze in a 3-hour visit to the doctor, honestly! Super easy, useful, inexpensive, and what a time saver too! Keep it up!”
At the risk of sounding overconfident, I wasn’t surprised. Of course, it always feels good to know that the product you are building and constantly aspiring to improve, is helping people and making their lives easier. It’s just that at this point we’ve come to expect such feedback. We knew for a fact that Healee was saving considerable amounts of time, for patients and doctors alike.
Nevertheless, the conversation I had with my friend got me thinking. Yes, what he told me was by far the norm, rather than an isolated appraisal. We’ve been hearing pretty much the same story from individual patients literally every day.
On the other hand, though, I would occasionally come across rather critical opinions doubting the merit and usefulness of telemedicine as a whole. In most cases, these opinions would not come as individual patient stories based on first-hand experience, but analyses or studies examining the concept of telemedicine, in general.
Criticism would mostly focus on two main problems, both reportedly undermining the potential for telemedicine to save time and money: overutilization and subpar quality of care.
To see whether and how these problems impact telemedicine, we need to go into deeper detail and closely analyse each of them.
Increased convenience > overutilization?
An assessment carried out by the RAND Corporation in 2017 claimed that in reality telemedicine doesn’t save time and money because the increased convenience it creates for patients often results in higher utilization, which eventually takes more time and costs more than in-person care would have.
According to the study, in-person visits among telemedicine users hardly decreased, meaning that 88% of the online visits were additive (visits that would not have occurred otherwise), with only 12% replacing in-person visits.
In other words: if people have access to telemedicine, they would use it. And then, in most cases, would go to see a doctor in person. At first glance, this looks plausible, right? The study, however, overlooks a couple of important aspects that actually make all the difference.
First and foremost, it doesn’t take into account the positive impact that this increased utilization has on prevention, especially in the long run. If these extra visits help doctors to diagnose a disease early on and thus prevent a more serious condition, patients will stay out of the hospital. This not only considerably raises quality of care and life, but also creates savings of time and money, which more than makes up for the initial cost of the extra visits.
Although released in 2017, the study used data on phone visits, gathered between 2011 and 2013. The changes in telehealth technology since then, and more importantly, the increased patient adoption and trust, render the data somewhat obsolete. People are now much more likely to turn to telemedicine as a valid substitute for an in-person visit.
Last but not least, the study did not consider the fact that on a like-for-like basis, telemedicine visits are considerably cheaper than in-person visits. This is only natural: with telemedicine, prices do not need to reflect a provider and a facility component, effectively resulting in cost savings not just for patients, but for doctors too.
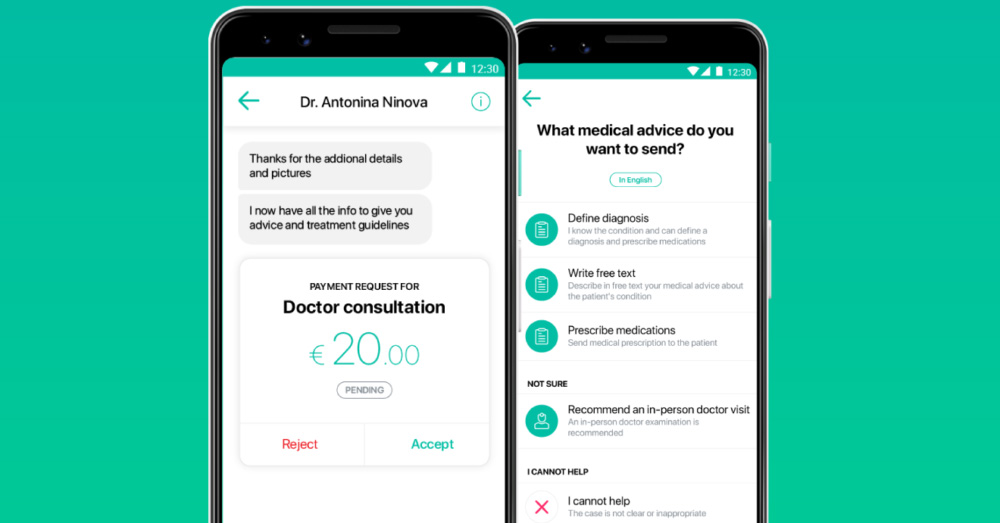
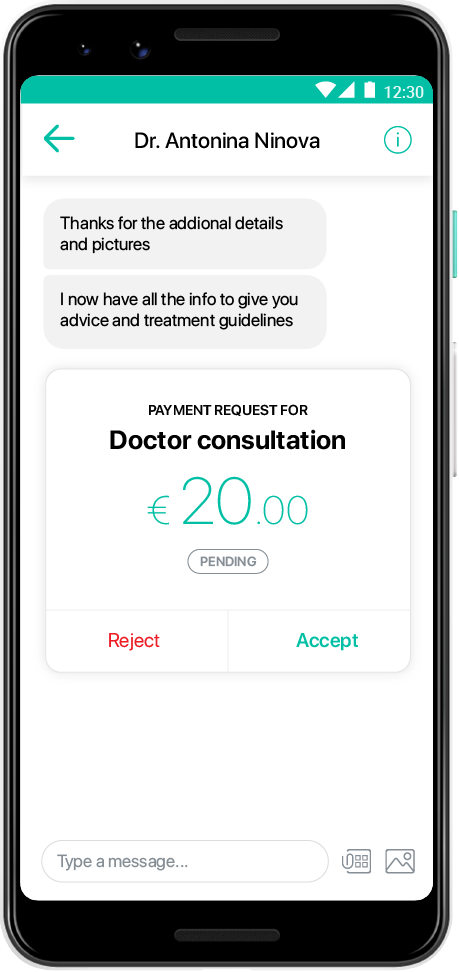
Indeed, our observations show that the great majority of doctors offer online consultation prices that are lower than prices for in-person visits. In light of that, it’s very important that telehealth platforms leave it to doctors and hospitals to define their online consultation prices.
Telemedicine = lower quality of care?
Another relatively widespread notion is that with telemedicine, quality is inevitably lower, due to the lack of face-to-face contact and physical examination. Hence, patients may often need to follow up with an in-person visit, which eventually leads to wasted time and higher costs.
This criticism mostly comes in the form of an opinion some people have about telemedicine and quality of care, in general. Studies or analyses in that direction are relatively scarce. An exception is a study published in March 2019 that claimed that doctors providing online consultations to patients with respiratory infections were more likely to unnecessarily prescribe antibiotics.
Details do matter
In any case, the criticism that telemedicine leads to lower quality of care is a little too generic. Details do make all the difference. The success of an online consultation heavily depends on a variety of factors, among which, most notably, the speciality and the case at hand.
In a number of specialities, studies have demonstrated that telehealth can be at least as effective, and sometimes even more effective than in-person care.
Dermatology
Teledermatology has been shown to increase patient satisfaction, save time and reduce costs by providing faster access to consultation as opposed to in-person visits, for specific populations.
Psychiatry
According to a 2018 policy update of the American Psychiatric Association, the use of live video sessions is a validated and effective approach, and a legitimate component of delivering mental health services, in a reliable, affordable and time saving manner. Equally importantly, telepsychiatry is superior to in-person care in helping reduce the stigma experienced by people with mental health disorders.
Endocrinology, OBGN
In some specialities, like endocrinology and gynecology, in certain cases involving the need for patient monitoring, telemedicine helps cut costs, and achieve levels and quality of patient follow-up that can never be attained if only in-person care were available.
Of course, telemedicine cannot always help save time and money, simply because in some cases, it is not a viable approach. There are situations where a patient case is best addressed with an in-person consultation. Doctors should rely on the telehealth platform they are using to be able to quickly and easily handle such cases, and notify patients if they need a physical examination.

To think that telemedicine can be universally applied, regardless of the underlying details, is to miss the point. The objective is not and will never be to replace face-to-face communication between doctors and patients. Instead, telemedicine is meant to provide access to care in situations such as my friend’s. A tool that complements in-person care, helps save time and money, and makes the lives of both patients and doctors easier.