
In the ever-evolving landscape of healthcare, patient access has emerged as a pivotal factor in delivering high-quality care. This rings especially true in the realm of mental healthcare, where timely and high-quality access to care can make a substantial difference in treatment outcomes and overall well-being.
As mental healthcare leaders, you’re undoubtedly familiar with the challenges associated with providing efficient and equitable access to mental health services. From stigma and limited awareness to geographical and socioeconomic barriers hindering accessibility, prolonged wait times for appointments, and intricate diagnostic and treatment landscapes, the delivery of mental care services has long been suboptimal.
Fortunately, technology has stepped up to the plate, offering innovative solutions to bridge the gap between consumer expectations and the current state of mental health care access. In this article, we’ll delve into the transformative power of patient access software and how it can revolutionize the delivery of mental health care.
Understanding the Importance of Patient Access in Mental Healthcare
Patient access refers to the ease and ability of patients to obtain timely and appropriate medical care and healthcare services. It encompasses the entire process of a patient seeking and receiving healthcare, from patient intake and scheduling appointments to receiving necessary treatments. Patient access is not only about the physical availability of healthcare facilities but also includes factors like geographic location, appointment scheduling, wait times, affordability, and the overall patient experience.
Efficient patient access is crucial to ensuring that individuals can receive the care they need in a timely manner, which is especially important for conditions that require prompt attention, such as acute illnesses or certain mental health crises. Achieving equitable patient access means that all individuals, regardless of their background, location, or socioeconomic status, should have an equal opportunity to access healthcare services without facing unnecessary barriers.
As you can see, patient access isn’t just a buzzword; it’s a critical cornerstone of effective healthcare delivery. When it comes to mental health care, patient access has an even larger significance.
Quick and convenient access to mental health services is essential for tailoring treatment plans, ensuring continuity of care, preventing crises, and combating stigma. Yet, the chasm between what patients expect and what the healthcare system currently offers is striking. According to the 2023 Ernst and Young Consumer Health Survey, access to care ranks as the foremost priority for U.S. respondents. Yet, only a mere 37% of healthcare consumers perceive their health system as delivering satisfactory access to care.
Challenges in the Current State of Mental Healthcare Access
Navigating the landscape of mental health care access is akin to a complex puzzle, with each piece representing a unique challenge. These hurdles, while diverse in nature, collectively contribute to the barriers that hinder timely and equitable access to mental health services. It’s crucial for mental healthcare leaders to dissect these challenges to pave the way for transformative solutions. Let’s take a look at the biggest obstacles when it comes to improving patient access to mental healthcare:
Administrative Complexities
One of the foremost challenges in the current state of mental health care access lies in the web of administrative complexities. From filling out extensive paperwork to coordinating insurance coverage, patients are often faced with a barrage of tasks that can deter them from seeking the care they need. These administrative burdens not only create unnecessary delays but can also exacerbate mental health conditions, emphasizing the urgency for streamlined solutions.
Geographical Barriers: A Struggle for Equitable Care
The geographical divide is another significant hurdle in mental health care access. In rural or underserved areas, access to specialized mental health services is often limited, forcing patients to travel long distances to receive care. Moreover, the maldistribution of mental health professionals means that even in urban centers, availability might be scarce. This geographic disparity not only strains patients but also perpetuates the notion that mental health care is a privilege accessible only to certain populations.
The Supply and Demand Gap
Picture a scenario where a patient, in desperate need of mental health care, is met with long wait times and inadequate provider matching. This scenario is a grim reality for many individuals seeking assistance.
More patients than ever are now pursuing mental healthcare, as indicated by AfPA’s report, which shows that approximately 53 million Americans now live with some form of mental illness. The impact of the COVID-19 pandemic has intensified this prevalence of mental health conditions, resulting in an unparalleled surge in the demand for mental health services.
This demand often outweighs the available supply of providers, leading to prolonged wait times that can exacerbate the patient’s condition. The mismatch between patient needs and provider availability is a significant challenge that requires innovative solutions.
The Stigma Surrounding Mental Health
The elephant in the room when discussing mental health care access is undoubtedly stigma. The pervasive societal prejudice surrounding mental health often discourages individuals from seeking help. Fear of judgment, discrimination, and a lack of understanding create a climate where mental health concerns are brushed aside or hidden. This stigma not only delays help-seeking but also perpetuates a culture where mental health care is relegated to the shadows.
Leveraging Technology for Enhanced Patient Access to Mental Healthcare
The National Institute of Mental Health outlines several ways technology can benefit both mental health patients and their providers:
Convenience: Enabling treatment at any time and place, whether it’s at home during late hours or a commute, catering well to those facing challenges attending in-person appointments.
Anonymity: Granting individuals the opportunity to receive treatment confidentially and privately from the comfort of their residences.
Introduction to Care: Serving as a positive initial step for individuals who have hesitated to engage in mental health care previously.
Cost-effectiveness: Enhancing affordability through applications that are free or more economical compared to traditional face-to-face care.
Wider Reach: Assisting mental health professionals in extending treatment to those in remote areas and addressing sudden surges in demand, such as post-natural disasters or traumatic incidents.
Engagement: Cultivating ongoing interest in therapy by offering care that is more engaging and accessible than traditional in-person methods.
24/7 Availability: Providing continuous monitoring and intervention support throughout the entire day.
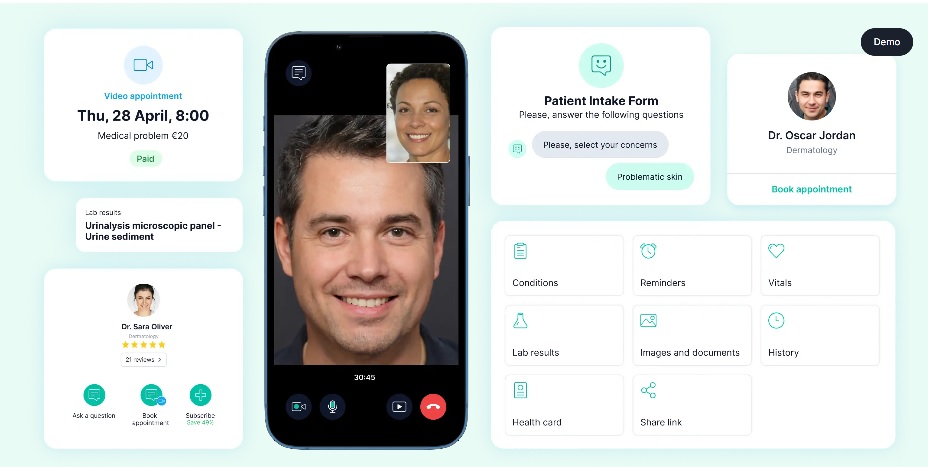
Because of all these advantages, mental health organizations are embracing innovative solutions to revolutionize the patient access landscape. Specialized software platforms are leading the charge, offering a range of features that streamline processes, boost efficiency, and most importantly, put patients at the center of care.
Let’s explore five key ways in which patient access software solutions can transform mental health care:
1. Sophisticated Patient Intake for Personalized Treatment
At the heart of efficient care delivery lies the patient intake process. Technology lends a helping hand by digitizing and optimizing this crucial step. Comprehensive patient information, including medical history, symptoms, and preferences, can be seamlessly collected and organized. This not only minimizes errors but also eliminates the need for time-consuming paperwork.
In the context of mental health, where diagnoses are vast and diverse, personalized patient intake becomes paramount. The software can be tailored to collect data specific to different mental health conditions, enabling providers to gain a deep understanding of each patient’s unique needs. Automated intake forms further facilitate personalized care plans, treatment eligibility assessments, and distinct patient journeys based on their condition.
Let’s take a detailed look at each of the benefits of a digital intake process for mental health:
Seamless Data Collection and Organization
Embracing technology means that healthcare providers can now seamlessly collect and organize comprehensive patient information in a fully HIPAA-compliant manner. Vital details such as medical history, symptoms, and patient preferences can be captured digitally, eradicating the errors that often arise from manual data entry. This transition not only enhances the accuracy of patient records but also significantly reduces the reliance on time-consuming paperwork. The result is a more efficient and error-free intake process, allowing healthcare professionals to focus on delivering quality care.
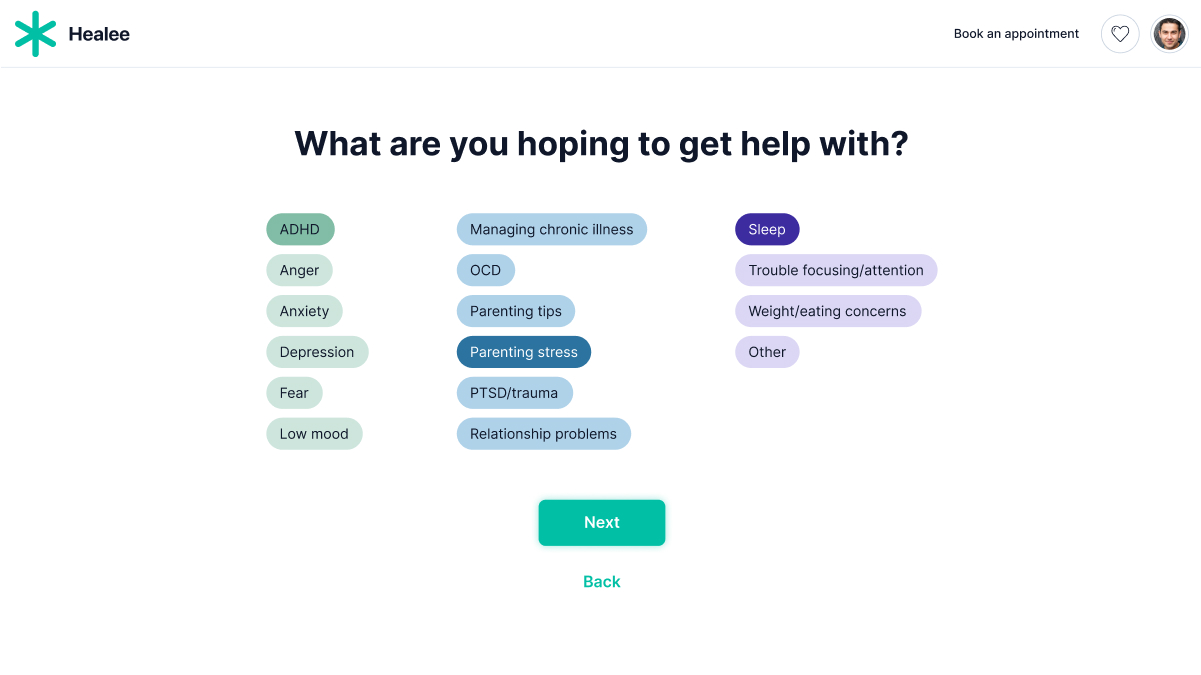
Personalized Approach to Mental Health
Within the realm of mental health, where diagnoses span a wide spectrum, the importance of a tailored patient intake process is magnified. Technological solutions can be specifically designed to gather data pertinent to various mental health conditions. This specialization empowers healthcare providers with a profound comprehension of each patient’s distinct requirements, enabling them to formulate more effective treatment plans.
Automated Intake Forms for Treatment Eligibility
One of the prime benefits of leveraging technology in patient intake is the automation of intake forms. These automated forms not only expedite the process but also offer a dynamic platform to assess treatment eligibility. As patients provide their information, the system can immediately assess their treatment eligibility based on established criteria (e.g. age, insurance coverage). Or, if for instance, you offer depression counseling services, the eligibility flow will allow the user to determine whether they are at risk for depression based on factors such as recent life events, emotional well-being, or family history.
Tailored Patient Journeys
The fusion of technology and patient intake also facilitates the creation of distinct patient journeys tailored to each user’s specific needs. In many cases, patient journeys are intertwined with the journeys of their caregivers. Technology enables healthcare providers to offer dedicated pathways for caregivers, acknowledging their crucial role and providing them with the resources they need to offer optimal support.
2. Robust Patient-Provider Matching to Improve Patient Outcomes
Well-designed patient-provider matching is the next critical step to ensuring good access to mental health care. Smart patient access platforms take the guesswork out of pairing patients with the right providers. Provider specialization, availability, and patient preferences are all taken into account to ensure optimal matches. This not only enhances patient outcomes but also maximizes provider expertise. Given the spectrum of mental health specialists and patient needs, this feature proves invaluable. Tailored access to a dedicated team of professionals can significantly elevate patient experiences and outcomes. The robust patient-provider matching capabilities of patient access software can bring a number of benefits for mental healthcare organizations, including:
Streamlined Matching Process
Traditional methods of assigning patients to providers often rely on manual coordination, which can leave room for inefficiencies and mismatches. With the advent of smart patient access platforms, the matching process becomes more streamlined and data-driven. These platforms leverage a wealth of patient data, provider specialization information, and availability schedules to make well-informed matches. This data-driven approach minimizes the guesswork, ensuring that patients are connected with providers who possess the expertise and availability to address their specific needs.
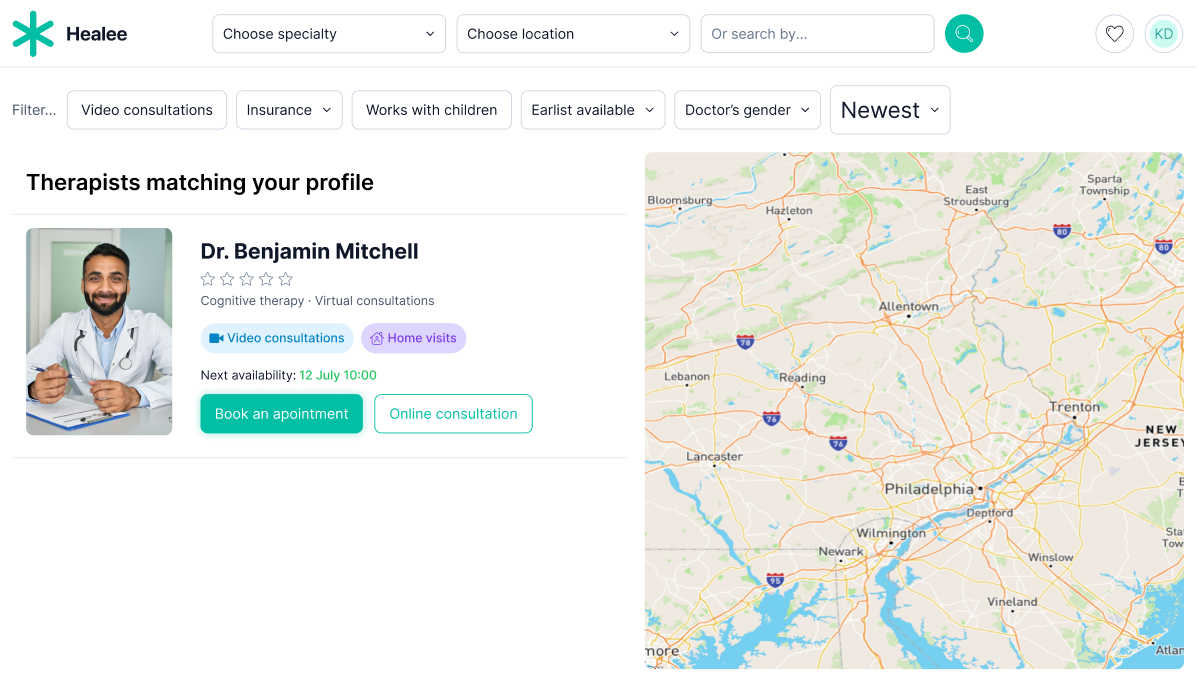
Personalized Matching Criteria for Better Treatment
The beauty of technology-enabled patient-provider matching lies in its ability to personalize the criteria for pairing patients and providers. Beyond just availability and location, these platforms consider patient preferences and provider specializations. Patients can express their preferences for a certain gender, language, or treatment approach, and these preferences are factored into the matching algorithm. Moreover, the platforms take into account the specific areas of expertise that providers offer, ensuring a more tailored and effective therapeutic relationship.
In the realm of mental health, where the nuances of patient-provider compatibility can significantly impact the effectiveness of treatment, robust patient-provider matching proves to be a game-changer. Patients struggling with different mental health conditions require unique approaches. Smart matching platforms consider these intricacies, ensuring that patients are paired with providers who have the experience and knowledge necessary to address their specific challenges.
3. Self-Scheduling for Timely and Convenient Access to Care
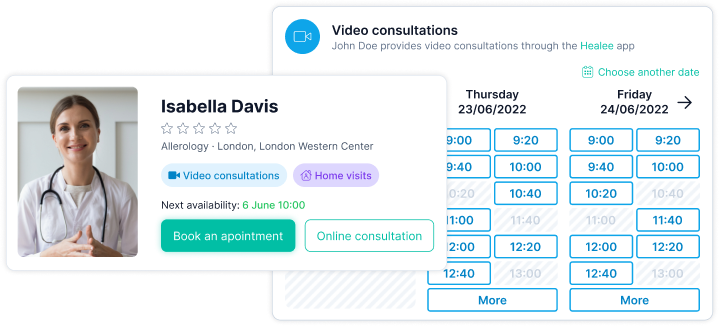
The evolution of healthcare systems is marked by a shift toward patient-centered experiences, and one of the key facets of this transformation is the integration of self-scheduling platforms. These innovative solutions revolutionize the way patients access care, granting them the autonomy to schedule appointments at their convenience. By eliminating the hassles of traditional appointment booking, self-scheduling platforms dramatically reduce wait times and ensure timely access to essential healthcare services. This feature of patient access software holds immense significance, especially in the realm of mental health, where the effectiveness of treatment is closely tied to timely interventions.
Let’s take a closer look at each of the benefits of self-scheduling when it comes to mental health:
Streamlined Appointment Booking
The traditional approach to appointment scheduling often involves a series of phone calls, potential back-and-forth conversations, and limited availability options. Self-scheduling platforms streamline this process by presenting patients with real-time availability, allowing them to select appointment slots that align with their schedules. This not only reduces the administrative burden on healthcare staff but also empowers patients to take control of their healthcare journey.
Empowerment Through Autonomy
Empowering patients to manage their own healthcare journey is a cornerstone of patient-centered care. Self-scheduling platforms exemplify this empowerment by placing the scheduling process in the hands of patients themselves. Patients can access the platform online or via mobile devices, selecting appointment times that suit their daily lives. This autonomy not only enhances patient satisfaction but also contributes to higher engagement levels.
Reducing Wait Times
In the context of healthcare, wait times can be a source of frustration for both patients and providers. Self-scheduling platforms play a pivotal role in alleviating this issue by optimizing appointment availability. Patients can quickly see open slots and secure appointments without the need for lengthy phone calls or email exchanges. This efficiency not only benefits patients seeking care but also ensures that healthcare providers can optimize their schedules and allocate resources more effectively.
Timely Access to Mental Health Care
The importance of timely access to care is particularly pronounced in mental health. Swift interventions can make a significant difference in managing and improving mental health conditions. Self-scheduling platforms break down barriers to access by enabling patients to secure appointments when they need them the most. This timeliness enhances the effectiveness of treatment, helping individuals navigate their mental health challenges with the right support.
Combating Missed Appointments
Persistent and costly, patient no-shows pose an enduring issue for healthcare systems. Based on statistics, the healthcare industry faces an estimated annual loss of over $150 billion due to these missed appointments.
These significant numbers have far-reaching implications for medical practices, resulting in an average yearly loss of $150,000 due to appointments that patients fail to attend. Moreover, each unfilled appointment slot amounts to around $200 in lost revenue for physicians. What is more, according to research, mental health patients are more likely to miss appointments. All of this highlights the pressing need for effective strategies that can reduce the occurrence of no-shows, ultimately leading to an improvement in patient engagement.
Self-scheduling platforms address this challenge by incorporating automatic notifications and reminders. Patients receive alerts via email, SMS, or app notifications, serving as gentle prompts for upcoming appointments. This proactive approach drastically reduces no-show rates, ensuring that patients attend their appointments as scheduled.
4. Calendar Management to Balance Availability for Different Appointment Types
The intricacies of mental health care demand efficient calendar management. The complexities inherent to mental health care necessitate a dynamic scheduling approach that can accommodate varying appointment types, durations, and therapeutic modalities. In response to this demand, modern software solutions step in to simplify and optimize the scheduling process, offering a suite of features that empower healthcare providers to allocate their time wisely and ensure the optimal utilization of resources.
Simplifying Appointment Scheduling
Traditional paper-based scheduling systems are often prone to errors and inefficiencies, especially in the context of mental health care. Modern software solutions revolutionize this process by providing intuitive interfaces that allow providers to seamlessly schedule appointments of different types and durations. Whether it’s a brief check-in or an in-depth therapy session, the software enables providers to allocate the appropriate amount of time for each appointment, ensuring a balanced and manageable schedule.
Preventing Overbooking and Underutilization
The intricacies of mental health care necessitate a delicate balance between patient needs and provider availability. Patient access software with calendar management capabilities addresses this challenge by offering real-time insights into provider schedules and appointment availability. By taking into account the varying lengths of appointments and the time required for documentation, the software helps prevent overbooking, ensuring that providers can dedicate their full attention to each patient. Simultaneously, it guards against underutilization of resources by optimizing the allocation of time slots.
Tailored Solutions for Mental Healthcare
Mental health care is highly individualized, with different patients requiring diverse care modalities and frequencies of appointments. Calendar management software acknowledges this diversity by offering customizable solutions. Providers can also create individual accounts for patients and their dependents, tailoring appointment schedules to their specific needs. This flexibility not only enhances patient experiences but also enables providers to offer more personalized and effective care plans.
Recurring Appointments and Follow-Up Care
Follow-up care is integral to the continuity of mental health treatment. Calendar management software provides the functionality to schedule recurring appointments, streamlining the process of securing regular check-ins and therapy sessions. This feature is particularly valuable for patients requiring ongoing support, ensuring that they receive consistent care and monitoring as part of their treatment plans.
5. Telehealth Capabilities to Increase Convenience and Flexibility
The integration of telehealth capabilities has ushered in a transformative era in mental health care delivery. This technological advancement offers a multitude of benefits, from enhanced convenience and flexibility to expanded accessibility and improved continuity of care. With the ability to provide remote therapy sessions and consultations, telehealth has revolutionized the landscape of mental health care, addressing various challenges and opening doors to novel opportunities.
Breaking Geographical Barriers
Telehealth serves as a game-changer in mental health care delivery by transcending traditional geographical boundaries. Remote therapy sessions and consultations break down the barriers imposed by travel constraints and distance limitations. Patients no longer need to factor in travel time, making it easier to prioritize their mental health and adhere to their treatment plans. This convenience is particularly valuable for individuals with busy schedules or mobility challenges.
Enhancing Treatment Adherence and Comfort
The comfort and privacy of one’s own space can contribute significantly to the effectiveness of mental health care. Telehealth allows patients to engage in therapy sessions from the comfort of their homes, reducing the potential anxiety associated with in-person visits. The increased comfort level can lead to improved patient engagement, as individuals are more likely to share openly and engage actively in their treatment process.
Overcoming Stigma
Telehealth offers a discreet and confidential avenue for seeking mental health care. The stigma often associated with mental health challenges can deter individuals from seeking help. By providing remote care options, telehealth allows patients to access the support they need without drawing attention or facing potential judgment. This confidentiality fosters an environment where patients feel safe to discuss their concerns openly.
Expanding Access to Underserved Areas
One of the most significant advantages of telehealth is its ability to bridge the gap in access to mental health care services. Remote and underserved areas often lack the availability of specialized mental health professionals. Telehealth extends care beyond urban centers, ensuring that individuals in rural or remote locations can access high-quality mental health services without the need for extensive travel.
Continuity of Care and Crisis Management
Telehealth contributes to the seamless continuity of care, even in times of crisis. Whether it’s a sudden change in circumstances or a natural disaster, telehealth enables mental health care providers to maintain contact with their patients. This uninterrupted care delivery is vital in maintaining stability and preventing setbacks during challenging times.
Summary
The significance of patient access cannot be understated, particularly within the realm of mental health. The journey to equitable and efficient mental healthcare access has been fraught with challenges, from stigma and geographical barriers to supply-demand imbalances. However, the infusion of technology, specifically patient access software, is propelling the transformation of mental health care delivery.
Patient access software is not just a technological innovation; it is a revolution in how mental health care is accessed, provided, and experienced. This software empowers mental healthcare providers to streamline administrative processes, match patients with the right providers, offer self-scheduling capabilities, manage calendars effectively, and provide telehealth solutions. These transformative functionalities address many of the long-standing challenges that have hindered timely and comprehensive mental health care.
As healthcare leaders embrace patient access software solutions, they are paving the way for a future where personalized treatment plans are crafted from the moment of patient intake, where every individual is matched with a provider who suits their unique needs, where self-scheduling promotes autonomy and reduces wait times, where calendars are optimized for efficient care delivery, and where telehealth ensures access to quality care regardless of geographical barriers.
This transformative journey is not only about embracing technology; it’s about humanizing healthcare. Patient access software enables mental healthcare to become more patient-centered, efficient, and accessible. It reduces the administrative burden on providers, improves treatment outcomes, enhances patient satisfaction, and combats the pervasive stigma surrounding mental health.
By harnessing the power of patient access software, mental healthcare is stepping into a new era that gives patients the tools to proactively manage their mental health, and allows providers to focus on what matters most – delivering effective care. The path ahead is clear: mental healthcare’s transformation through patient access software is shaping a future where access to quality care is a right, not a privilege, and where the journey to mental wellness is both supported and empowered.
Discover the secrets to choosing and effectively launching your patient access software with Healee’s in-depth Buyer’s Guide. Download for free here.