Patient access has long been hindered by various barriers, including cumbersome administrative processes and paperwork, provider shortages, and a gap between supply and demand due to suboptimal patient-provider matching. The advent of patient access technology, however, has empowered medical groups with the tools to dramatically improve patient inclusion.
Patient self-scheduling is one of the most crucial components of enabling better patient access. By putting the power of appointment booking directly into the hands of patients, self-scheduling offers a promising way to overcome patient access barriers, improve patient satisfaction and boost resource utilization.
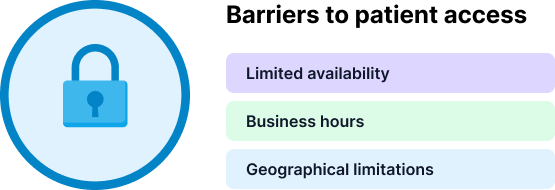
What are the barriers to patient access for medical groups
Patient access refers to the ability of individuals to obtain timely and appropriate healthcare services. It encompasses the ease with which patients can enter the healthcare system, schedule appointments, receive necessary treatments, and access healthcare facilities and providers. Patient access involves various aspects, including physical accessibility, availability of healthcare services, affordability, and the elimination of barriers that may prevent or delay individuals from receiving the care they need.
In essence, patient access aims to ensure that individuals have the opportunity to receive healthcare services when they require them, regardless of factors such as location, socioeconomic status, language barriers, or administrative complexities. Improving patient access is key to promoting equitable healthcare delivery, enhancing patient outcomes, and reducing health disparities within populations.
The barriers to patient access can vary and include:
Limited availability
Limited appointment availability can significantly delay access to necessary healthcare. Overburdened healthcare systems and a shortage of healthcare providers contribute to this issue. According to a report by Merritt Hawkins, the average time to get an appointment scheduled in 2022 was 26 days. During this long period of time, a patient’s condition can worsen or the patient may explore alternative provider choices. Long wait times are both dangerous to the patient and could increase the cost of healthcare.
By granting patients the ability to directly schedule appointments, patient self-scheduling eliminates the dependence on traditional phone-based or in-person booking systems, which can often be time-consuming and prone to human error. In addition, by allowing patients to select from open slots, self-scheduling minimizes gaps in appointment schedules, ensuring more efficient use of healthcare providers’ time while decreasing time to appointment. Strong patient self-scheduling solutions also allow for cadenced follow-up appointments by patients to eliminate the need to repeatedly schedule appointments for ongoing care and eliminate the risk of unavailability.
Business hours
A typical medical practice operates between 8:00 am and 5:00 pm, or a similar schedule. The limited business hours restrict patient access and make it especially difficult for people with untypical work schedules to set an appointment. Often, such patients choose to put off care for as long as possible.
By implementing self-scheduling, healthcare providers can extend their availability beyond traditional office hours, offering patients increased flexibility and access to appointments. Given that as much as 51% of appointments are self-scheduled outside of office hours, self-scheduling plays an important role in eliminating this barrier to patient access.
Geographical limitations
Patients living in remote or rural areas may face challenges in accessing healthcare due to the limited availability of healthcare facilities and specialists.
By granting patients the autonomy to schedule their own appointments, it not only empowers them to proactively seek necessary care but also effectively addresses the issue of patient no-shows that stem from transportation-related challenges. With self-scheduling, patients gain increased visibility into available appointment slots and have the flexibility to choose a date and time that best accommodates their individual schedules.
That, coupled with a robust virtual care offering, can dramatically improve access to care by allowing patients in remote or underserved areas to book virtual appointments at their convenience, reducing the need for long-distance travel.
What is patient self-scheduling
Patient self-scheduling enables patients to book their healthcare appointments online using a portal, website, or mobile application from anywhere, at any time and without staff interaction. Instead of relying on traditional methods such as phone calls or in-person scheduling, this technology allows patients to take control of their healthcare journey by providing them with greater flexibility, convenience, and accessibility when it comes to securing medical appointments. By eliminating the need for time-consuming phone calls and enabling 24/7 scheduling, patient self-scheduling enhances efficiency for both patients and healthcare providers, ultimately improving the overall patient experience.
A scoping review that looked at 30 scientific texts discovered that patient self-scheduling comes with impressive benefits for healthcare organizations. Implementing scheduling tools brings a 25% decrease in staff dedicated to scheduling, with yearly savings of $170,000 for medical practices. The findings also report that up to 51% of medical appointments are scheduled outside of office hours, leading to improved accessibility and customer satisfaction.
The researchers concluded that the advantages of automated patient self-scheduling span from better organizational efficiency, cost reduction, and more effective allocation of resources to higher patient satisfaction, loyalty, accountability, and attendance.
What makes patient self-scheduling so effective? Its power to eliminate the barriers to patient access.
How patient self-scheduling helps clinical ops and providers
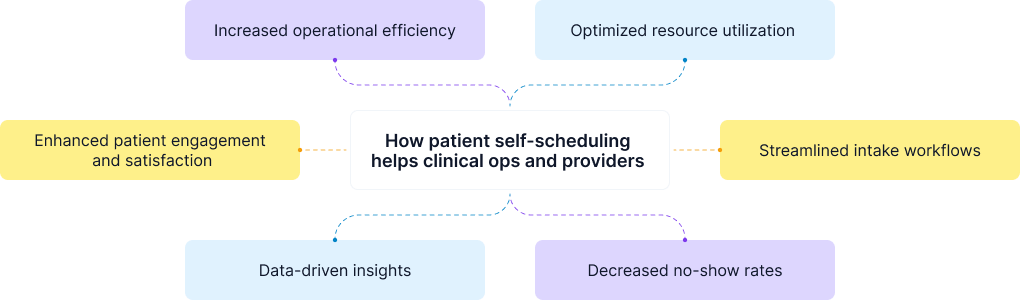
Patient self-scheduling offers numerous benefits to healthcare staff and operations, contributing to improved efficiency, productivity, and overall satisfaction. Here are some ways patient self-scheduling dramatically improves healthcare staff and operations:
Increased operational efficiency
Patient self-scheduling reduces the administrative burden on healthcare staff by eliminating the need for manual appointment booking. This frees up valuable time for staff to focus on other critical tasks, such as patient care and clinical responsibilities.
When patients schedule their appointments independently, there is no need for staff intervention. However, when appointments are scheduled over the phone, it typically takes staff an average of 8 minutes. This amounts to a significant allocation of staff time towards phone calls that do not contribute to patient satisfaction or efficiency.
The time saved by implementing self-scheduling in comparison to traditional scheduling results in substantial cost savings. In fact, for every 100 appointments booked through self-scheduling, you can save the equivalent of one full-time employee. In other words, only by having six self-scheduled appointments per day, you can offset the cost of implementing a self-scheduling solution. And each subsequent self-scheduled appointment not only adds to the savings but also generates an additional $1 for your practice.
Optimized resource utilization
Patient self-scheduling allows for better utilization of available time slots. Patients can book 24/7 and can reschedule or cancel their appointments, which avoids unnecessary phone calls and last-minute cancellations and results in availability that is always up to date. Self-scheduling also reduces gaps in the working day and eliminates errors and double-bookings, maximizing the productivity of healthcare providers.
Streamlined intake workflows
A robust self-scheduling platform incorporates eligibility forms and intake questionnaires, which allow medical groups to optimize their patient flow and improve data accuracy.
Eligibility forms streamline the patient journey by offering pre-defined intake questionnaires or medical forms that can be placed at various stages or trigger events, simplifying registration and triage. Provider tags allow for customized settings on provider profiles, ensuring better patient-provider matching based on specific criteria such as preferences, requirements, and suitability. Additionally, easy self-service access and simplified intake workflows through intake questionnaires reduce errors and collect essential patient information before the appointment. This combination of patient empowerment and efficient data collection contributes to a well-managed and seamless care workflow.
Decreased no-show rates
Robust patient self-scheduling platforms include automated appointment reminders, which help reduce no-show rates. Patients receive timely reminders through various channels (e.g., email, SMS), increasing the likelihood of keeping appointments and reducing missed opportunities for care.
Research by Mayo Clinic looked at 1,099 patients who self-scheduled their appointments over one year. The study showed that self-scheduled doctor visits had fewer no-shows, cancellations, and reschedulings than those that were scheduled by staff.
Data-driven insights
Patient self-scheduling systems generate valuable data on appointment patterns, patient preferences, and scheduling metrics. Medical groups can analyze this data to gain insights into patient behavior, optimize scheduling processes, and make informed decisions to improve service delivery and resource allocation.
Enhanced patient engagement and satisfaction
By giving patients the ability to self-schedule, medical groups empower individuals to take an active role in managing their healthcare. Patients have greater control over their healthcare journey, which can lead to increased patient engagement, better adherence to treatment plans, and improved health outcomes.
Patient self-scheduling offers convenience, flexibility, and control to patients, resulting in higher levels of satisfaction. Patients appreciate the ability to choose appointment times that align with their preferences and needs. Improved satisfaction leads to a better overall patient experience and a positive perception of the healthcare provider.
Why you may see resistance to patient self-scheduling

Patient self-scheduling appears to be an obvious choice, considering its benefits of meeting patient preferences and alleviating staff workload. It’s easy to understand why it’s widely embraced. However, it’s essential to acknowledge that resistance can arise when implementing new systems, particularly in the healthcare sector.
The process of matching patients and providers is extremely complex and requires setting a number of scheduling rules and constraints (including appointment types, lengths, need for specialized equipment, need to preliminary inform the patient, allowing for complex appointment types or care modalities, patient eligibility, provider expertise, preferences and suitability, and patient prioritization). This is why medical groups are worried a self-scheduling solution can hardly fit their operations and workflows.
By recognizing and understanding these challenges and concerns, we can pave the way for the successful adoption of digital scheduling solutions, which fulfill crucial needs within the medical group.
Reluctance to change
Implementing patient self-scheduling requires a shift in the traditional appointment booking process. Ops and clinical staff may be resistant to change or hesitant to adopt new technologies and systems, especially if they have been accustomed to existing workflows for a long time.
Fear of increased workload
Some staff members may worry that patient self-scheduling could lead to an increased workload or create additional administrative tasks. They may anticipate the need to manage more appointments, handle patient inquiries, or address scheduling conflicts that arise from the self-scheduling system.
Concerns about patient competency
There may be concerns that patients might struggle using the self-scheduling platform or make errors while booking appointments. Ops and clinical staff might worry that patients could inadvertently select incorrect services, overbook or double-book appointments, or fail to provide essential information during the scheduling process.
Apprehension about loss of control
Ops and clinical staff are accustomed to managing the appointment scheduling process to ensure smooth operations and optimal patient care. With patient self-scheduling, they may feel a loss of control or worry about potential disruptions to their established routines and workflows.
Technological challenges
Implementing patient self-scheduling requires appropriate technological infrastructure and integration with existing systems. Ops and clinical staff may be skeptical about the reliability, usability, and security of the self-scheduling software or platforms. Concerns about technical glitches, data breaches, data interoperability, or system downtime may contribute to resistance.
Communication and patient relationship concerns
Some staff members may fear that patient self-scheduling could hinder effective communication and relationship-building with patients. They might worry that reducing direct interaction during the scheduling process could limit opportunities to address patient inquiries, provide personalized guidance, or assess the urgency or appropriateness of appointments.
Addressing these concerns and resistance is crucial to successfully implementing patient self-scheduling. Proper training, clear communication about the benefits, addressing staff members’ apprehensions, involving them in the planning process, and providing ongoing support can all help alleviate resistance and ensure a smooth transition to self-scheduling practices. Emphasizing the positive impact on efficiency, patient satisfaction, and workload distribution can also help staff members recognize the value of patient self-scheduling.
Summary
Ensuring timely, consistent, and convenient patient access is becoming increasingly crucial for provider groups as they strive to foster patient loyalty and operational efficiency. However, achieving this goal requires a shift in the mindset regarding how organizations provide access to care. To maximize the value of patient self-scheduling, medical groups need to address concerns and resistance to adoption, emphasizing the importance of staff engagement and proper training. While the current access process is often suboptimal in most organizations, it is possible to envision a robust access system that maximizes utilization, enhances income, and delivers an exceptional patient experience.
Patient self-scheduling technology has emerged as one of the key components of patient access solutions. By enabling patients to book appointments online at their convenience, self-scheduling improves operational efficiency and resource utilization and dramatically increases patient engagement, satisfaction, and loyalty.
To learn how Healee can help you launch your fully-branded patient scheduling solution in just a few weeks, request a personalized demo now.